• Do you have difficulty falling or staying asleep?
• Are you excessively sleepy during the day or fall asleep when you don't want to?
• Do you snore or have you been told that you snore loudly?
• Do you gasp for air or have you been told that you stop breathing during sleep?
• Do you experience uncomfortable sensations in the legs in the evening that are relieved by movement?
• Are you a restless sleeper or have you been told that you kick during sleep?
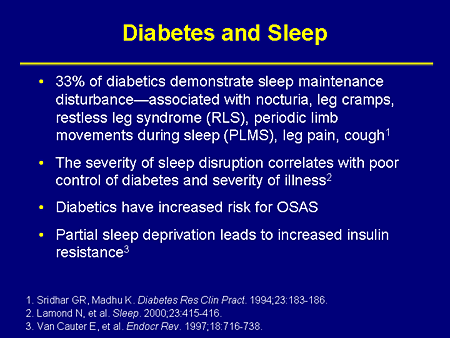
SLEEP disturbances are common and can be detrimental to the health, mood, and quality of life of people with diabetes. Sleep-disordered breathing, pain, restless legs syndrome, primary insomnia, and lifestyle factors all contribute to a high rate of sleep complaints in this population.
• Are you excessively sleepy during the day or fall asleep when you don't want to?
• Do you snore or have you been told that you snore loudly?
• Do you gasp for air or have you been told that you stop breathing during sleep?
• Do you experience uncomfortable sensations in the legs in the evening that are relieved by movement?
• Are you a restless sleeper or have you been told that you kick during sleep?
SLEEP disturbances are common and can be detrimental to the health, mood, and quality of life of people with diabetes. Sleep-disordered breathing, pain, restless legs syndrome, primary insomnia, and lifestyle factors all contribute to a high rate of sleep complaints in this population.
Because the etiology of poor sleep quality is often multifactorial and may shift over time, a careful evaluation for insomnia, sleep-disordered breathing, and restless legs syndrome should be an integral part of the routine care of patients with diabetes, say experts.
Generally, people with diabetes have poorer sleep than non-diabetics. Also, poor sleep has been proposed as a risk factor for developing the disease. Sleep disorders, such as obstructive sleep apnea, are more prevalent in people with type 2 diabetes. Therefore, it is not surprising that up to 71% of this population complain of poor sleep quality and high rates of hypnotic use.
Diabetes is worse when combined with insomnia symptoms. In fact, insomnia makes most medical diseases much worse in ways that are only just being found out and can chemically disrupt the body’s insulin balance enough to even be a root cause for certain types of diabetes, say experts.
Insomnia-Insulin Resistance Link
The loss of normal sleep hours or addition of sleep hours seems to undo the body’s chemistry and completely throw off-balance the blood glucose levels. Doctors don’t know for sure the exact chemistry behind this phenomenon outside of the observation. This underscores the importance of the sleep cycle chemistry.
In Knutson’s study, for example, among the diabetics, poor sleepers had 23% higher blood glucose levels in the morning, and 48% higher blood insulin levels. Using these numbers to estimate a person's insulin resistance, the researchers found that poor sleepers with diabetes had 82% higher insulin resistance than normal sleepers with diabetes.
Other studies have shown that chronic insomnia in healthy people can also instigate diabetes. Loss of sleep interrupts insulin balance—leads to insulin resistance—which in turn can lead to more severe medical problems and Type 2 diabetes.
Diabetes Management
Generally, people with diabetes have poorer sleep than non-diabetics. Also, poor sleep has been proposed as a risk factor for developing the disease. Sleep disorders, such as obstructive sleep apnea, are more prevalent in people with type 2 diabetes. Therefore, it is not surprising that up to 71% of this population complain of poor sleep quality and high rates of hypnotic use.
Diabetes is worse when combined with insomnia symptoms. In fact, insomnia makes most medical diseases much worse in ways that are only just being found out and can chemically disrupt the body’s insulin balance enough to even be a root cause for certain types of diabetes, say experts.
Insomnia-Insulin Resistance Link
In the largest study of its kind to establish a link between sleep and diabetes ‒ published in the June issue of Diabetes Care ‒ researchers have found that people with diabetes who sleep poorly have higher insulin resistance, and a harder time controlling the disease.
"Poor sleep quality in people with diabetes was associated with worse control of their blood glucose levels," says Kristen Knutson, PhD, assistant professor of medicine at the University of Chicago Medical Center and lead author of the study.
"People who have a hard time controlling their blood glucose levels have a greater risk of complications. They have a reduced quality of life. And, they have a reduced life expectancy," she explains in apress statement.
Multiple factors contribute to insomnia complaints in patients with diabetes, say Phyllis C Zee, and Erik Naylor in their expert columnin Medscape. In type 1 diabetes, rapid changes in glucose levels during sleep have been postulated to cause awakenings. For individuals with type 2 diabetes, sleep disturbances may be related to obesity or obesity-associated sleep disorders, such as sleep apnea.
Sleep-disordered breathing correlates highly with obesity in the diabetic population. A strong association also exists between obesity, impaired glucose tolerance, insulin resistance, and sleep-disordered breathing.
Furthermore, the severity of sleep-disordered breathing, as measured by the apnea-hypopnea index, correlates with the severity of glucose intolerance, insulin resistance, and diabetes. Although obstructive sleep apnea is the most common type of sleep-disordered breathing, central-type apneas and periodic breathing have been reported in patients with autonomic diabetic neuropathy.
The Chemistry of the Sleep-Wake Cycle
"Poor sleep quality in people with diabetes was associated with worse control of their blood glucose levels," says Kristen Knutson, PhD, assistant professor of medicine at the University of Chicago Medical Center and lead author of the study.
"People who have a hard time controlling their blood glucose levels have a greater risk of complications. They have a reduced quality of life. And, they have a reduced life expectancy," she explains in apress statement.
Multiple factors contribute to insomnia complaints in patients with diabetes, say Phyllis C Zee, and Erik Naylor in their expert columnin Medscape. In type 1 diabetes, rapid changes in glucose levels during sleep have been postulated to cause awakenings. For individuals with type 2 diabetes, sleep disturbances may be related to obesity or obesity-associated sleep disorders, such as sleep apnea.
Sleep-disordered breathing correlates highly with obesity in the diabetic population. A strong association also exists between obesity, impaired glucose tolerance, insulin resistance, and sleep-disordered breathing.
Furthermore, the severity of sleep-disordered breathing, as measured by the apnea-hypopnea index, correlates with the severity of glucose intolerance, insulin resistance, and diabetes. Although obstructive sleep apnea is the most common type of sleep-disordered breathing, central-type apneas and periodic breathing have been reported in patients with autonomic diabetic neuropathy.
The Chemistry of the Sleep-Wake Cycle
Since diabetics are sensitive to blood glucose levels and chemical balances in the body, it’s illustrative to explore just how detrimental disruptions in the sleep cycle can be. Studies have shown that diabetes worsens when adult sufferers sleep less than 6 hours per night or more than 9.
The loss of normal sleep hours or addition of sleep hours seems to undo the body’s chemistry and completely throw off-balance the blood glucose levels. Doctors don’t know for sure the exact chemistry behind this phenomenon outside of the observation. This underscores the importance of the sleep cycle chemistry.
In Knutson’s study, for example, among the diabetics, poor sleepers had 23% higher blood glucose levels in the morning, and 48% higher blood insulin levels. Using these numbers to estimate a person's insulin resistance, the researchers found that poor sleepers with diabetes had 82% higher insulin resistance than normal sleepers with diabetes.
Other studies have shown that chronic insomnia in healthy people can also instigate diabetes. Loss of sleep interrupts insulin balance—leads to insulin resistance—which in turn can lead to more severe medical problems and Type 2 diabetes.
Diabetes Management
Much of the challenge for diabetics is proper and long-term management of their diabetes. When the sleep-wake cycle is also mismanaged, so too is the diabetes. Like many other medical diseases and conditions, diabetes is sensitive to sleep disturbances. But insomnia, as a set of symptoms, is usually secondary to something else.
Insomnia is characterized in a number of ways: you could have problems going to sleep (sleep onset insomnia), problems waking up and going back to sleep (middle of the night insomnia), or waking up in the early dawn unable to return to sleep that night (terminal or late insomnia). Doctors can often associate particular patterns of insomnia such as these to particular medical problems.
Insomnia is rarely treated as a primary affliction. In most medical sectors it’s important to identify and diagnose insomnia for its implication in other problems, including depression, a common secondary illness to diabetes. As patients get older, the risk for depression escalates. Loss of a loved one, stress, anxiety and a range of other social disturbances can set in motion the symptoms for chronic insomnia. Loss of sleep makes for haywire blood sugar.
The Way Forward
Insomnia is characterized in a number of ways: you could have problems going to sleep (sleep onset insomnia), problems waking up and going back to sleep (middle of the night insomnia), or waking up in the early dawn unable to return to sleep that night (terminal or late insomnia). Doctors can often associate particular patterns of insomnia such as these to particular medical problems.
Insomnia is rarely treated as a primary affliction. In most medical sectors it’s important to identify and diagnose insomnia for its implication in other problems, including depression, a common secondary illness to diabetes. As patients get older, the risk for depression escalates. Loss of a loved one, stress, anxiety and a range of other social disturbances can set in motion the symptoms for chronic insomnia. Loss of sleep makes for haywire blood sugar.
The Way Forward
Knutson says the next step for researchers is to see if treating poor sleep can improve long-term outcomes and quality of life for diabetics. "For someone who already has diabetes, adding a sleep treatment intervention, whether it's treating sleep apnea or treating insomnia, may be an additional help for them to control their disease," she points out.
In fact, restoring a healthy amount of sleep may be as powerful an intervention as the drugs currently used to treat type 2 diabetes. "This suggests that improving sleep quality in diabetics would have a similar beneficial effect as the most commonly used anti-diabetes drugs," says Eve Van Cauter, PhD, professor of medicine and co-author of the study.
"For someone who already has diabetes, adding a sleep treatment intervention, whether it's treating sleep apnea or treating insomnia, may be an additional help for them to control their disease," feels Knutson.
Further investigation into which leads to the other – the chronic poor sleep or chronic insulin resistance – could improve the quality of life for people with type 2 diabetes. "Anything that we can do to help people improve their ability to control their glucose will help their lives in the long run," Knutson concludes.
"For someone who already has diabetes, adding a sleep treatment intervention, whether it's treating sleep apnea or treating insomnia, may be an additional help for them to control their disease," feels Knutson.
Further investigation into which leads to the other – the chronic poor sleep or chronic insulin resistance – could improve the quality of life for people with type 2 diabetes. "Anything that we can do to help people improve their ability to control their glucose will help their lives in the long run," Knutson concludes.