PREMATURE attributions of cause and effect should not be used to justify recommendations in favor of coffee drinking as beneficial to health, especially given the broad range of adverse effects attributable to caffeine.
More than 220 million people worldwide have diabetes and the links that have been revealed between diabetes and the consumption of caffeine beverages (especially coffee) are of monumental importance when it is acknowledged that more than 80% of the world's population consumes caffeine daily.
Caffeine Effects on Insulin Resistance
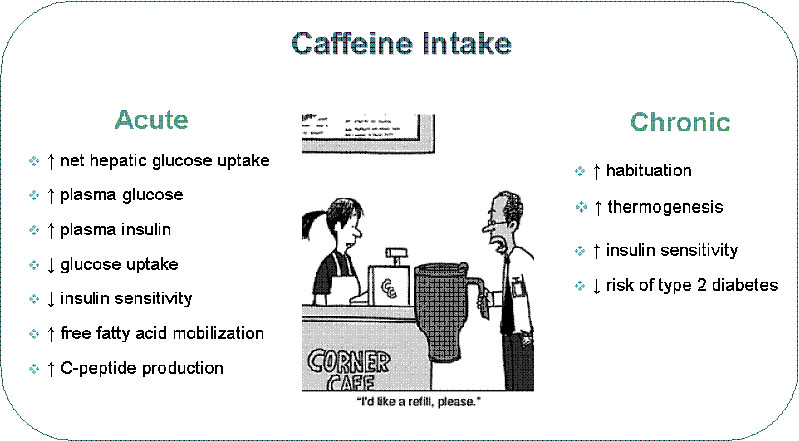
The effects of caffeine on glucose metabolism have been studied in both healthy and T2DM individuals. The studies of healthy adults demonstrate the impact of caffeine when glucose regulation has not been compromised.
These results relate most directly to caffeine's potential contributions to T2DM development, in those who are predisposed to the disease, and prevention. Studies of patients who have T2DM provide evidence of the potential clinical impact of caffeine on glucose management. Studies in both groups provide strong evidence that caffeine impairs glucose homeostasis through a transient increase in insulin resistance.
At least 17 studies were published between 1968 and 2010 describing the effects of caffeine on glucose metabolism in healthy nondiabetic adults. Most of the studies examined glucose and insulin responses to carbohydrate challenge. Glucose and insulin levels were measured first under fasting conditions and then repeatedly for several hours after administration of a standard dose of glucose or carbohydrate administered orally or by intravenous infusion (IV).
Of the 14 studies that used this challenge protocol, all but one found evidence of insulin resistance after caffeine administration, compared to placebo control. Insulin responses were significantly larger after caffeine, indicating that more insulin was required to dispose of the glucose.
Even though more insulin was secreted after caffeine, none of the studies observed smaller glucose responses. Indeed, some found that caffeine potentiated the postchallenge glucose responses as well. Those who calculated whole-body insulin sensitivity index (ISI) found that caffeine decreased this measure of insulin sensitivity.
Three other studies used a technique known as the hyperinsulinemic-euglycemic clamp to measure caffeine's effects on insulin sensitivity more directly. All three studies found that a moderate dose of caffeine significantly decreased glucose disposal compared to placebo control. These results provide specific evidence that caffeine produces an acute reduction in insulin sensitivity (increased insulin resistance) in healthy nondiabetic men and women.
Studies have investigated the impact of caffeine on glucose tolerance in patients who have T2DM. Because diabetic patients typically have smaller insulin reserves, ingestion of carbohydrate usually produces a sustained hyperglycemia.
Indeed a growing body of research suggests that caffeine disrupts glucose metabolism and may contribute to the development and poor control of type 2 diabetes. A review article in the inaugural issue of Journal of Caffeine Research examines the latest evidence, contradicting earlier studies suggesting a protective effect of caffeine.
In the lengthy review that cites 49 past and current research studies, James Lane of Duke University describes numerous studies that have demonstrated caffeine's potential for increasinginsulin resistance (impaired glucose tolerance) in adults that do not have diabetes, an effect that could make susceptible individuals more likely to develop the disease. In adults with type 2 diabetes mellitus (T2DM), studies have shown that the increase in blood glucose levels that occurs after they eat carbohydrates is exaggerated if they also consume a caffeinated beverage such as coffee. This effect could contribute to higher glucose levels in people with diabetes and could compromise treatment aimed at controlling their blood glucose.
In the lengthy review that cites 49 past and current research studies, James Lane of Duke University describes numerous studies that have demonstrated caffeine's potential for increasinginsulin resistance (impaired glucose tolerance) in adults that do not have diabetes, an effect that could make susceptible individuals more likely to develop the disease. In adults with type 2 diabetes mellitus (T2DM), studies have shown that the increase in blood glucose levels that occurs after they eat carbohydrates is exaggerated if they also consume a caffeinated beverage such as coffee. This effect could contribute to higher glucose levels in people with diabetes and could compromise treatment aimed at controlling their blood glucose.
More than 220 million people worldwide have diabetes and the links that have been revealed between diabetes and the consumption of caffeine beverages (especially coffee) are of monumental importance when it is acknowledged that more than 80% of the world's population consumes caffeine daily.
Caffeine Effects on Insulin Resistance
The effects of caffeine on glucose metabolism have been studied in both healthy and T2DM individuals. The studies of healthy adults demonstrate the impact of caffeine when glucose regulation has not been compromised.
These results relate most directly to caffeine's potential contributions to T2DM development, in those who are predisposed to the disease, and prevention. Studies of patients who have T2DM provide evidence of the potential clinical impact of caffeine on glucose management. Studies in both groups provide strong evidence that caffeine impairs glucose homeostasis through a transient increase in insulin resistance.
At least 17 studies were published between 1968 and 2010 describing the effects of caffeine on glucose metabolism in healthy nondiabetic adults. Most of the studies examined glucose and insulin responses to carbohydrate challenge. Glucose and insulin levels were measured first under fasting conditions and then repeatedly for several hours after administration of a standard dose of glucose or carbohydrate administered orally or by intravenous infusion (IV).
Of the 14 studies that used this challenge protocol, all but one found evidence of insulin resistance after caffeine administration, compared to placebo control. Insulin responses were significantly larger after caffeine, indicating that more insulin was required to dispose of the glucose.
Even though more insulin was secreted after caffeine, none of the studies observed smaller glucose responses. Indeed, some found that caffeine potentiated the postchallenge glucose responses as well. Those who calculated whole-body insulin sensitivity index (ISI) found that caffeine decreased this measure of insulin sensitivity.
Three other studies used a technique known as the hyperinsulinemic-euglycemic clamp to measure caffeine's effects on insulin sensitivity more directly. All three studies found that a moderate dose of caffeine significantly decreased glucose disposal compared to placebo control. These results provide specific evidence that caffeine produces an acute reduction in insulin sensitivity (increased insulin resistance) in healthy nondiabetic men and women.
Studies have investigated the impact of caffeine on glucose tolerance in patients who have T2DM. Because diabetic patients typically have smaller insulin reserves, ingestion of carbohydrate usually produces a sustained hyperglycemia.
The effects of caffeine on this postprandial hyperglycemic response was first studied in 1967, when the observation was made that two cups of instant coffee (compared to hot water) exaggerated the rise in blood glucose that followed the IV injection of glucose solution.
This effect has been replicated in three more recent studies that tested the effects of double-blind administration of moderate doses of caffeine vs. placebo on glucose and insulin responses to carbohydrate challenge. The effects of caffeine were also studied in women who had gestational diabetes, a form of glucose dysregulation that can occur during pregnancy.
In all four studies, caffeine exaggerated the glucose and insulin responses to the carbohydrate challenge and decreased whole-body insulin sensitivity. These results confirm that caffeine increases insulin resistance in T2DM patients, as it does in nondiabetic patients. However, in T2DM patients, this effect also exaggerates the hyperglycemic response to carbohydrate.
Caffeine can impair glucose regulation in the real world as well as in the laboratory. An ambulatory study monitored glucose levels continuously for several days during the ordinary activities of a small group of T2DM coffee drinkers. The results provide evidence that caffeine impairs glucose regulation in the natural environment where caffeine is consumed, as it does in the laboratory.
Mechanism
In general, caffeine is thought to produce its widespread physiological effects through actions as a potent antagonist for adenosine receptors both centrally and peripherally. One hypothesis is that caffeine impairs glucose metabolism through the release of stress hormones, especially epinephrine and cortisol. Evidence from two human studies supports this hypothesis.
One study found that the drug propranolol, used to block the beta-adrenergic actions of epinephrine, abolished caffeine's exaggeration of the postprandial insulin response and the reduction of whole-body insulin sensitivity.
A second study found that caffeine had no effects on glucose tolerance in a group of adults with tetraplegia, who did not produce increased epinephrine in response to caffeine. Both studies suggest that epinephrine could mediate caffeine's effects on glucose and insulin resistance.
However, a study that directly compared caffeine with high- and low-dose epinephrine infusions for their effects on insulin sensitivity found that caffeine did not raise epinephrine levels high enough to fully account for effects on glucose metabolism.
This effect has been replicated in three more recent studies that tested the effects of double-blind administration of moderate doses of caffeine vs. placebo on glucose and insulin responses to carbohydrate challenge. The effects of caffeine were also studied in women who had gestational diabetes, a form of glucose dysregulation that can occur during pregnancy.
In all four studies, caffeine exaggerated the glucose and insulin responses to the carbohydrate challenge and decreased whole-body insulin sensitivity. These results confirm that caffeine increases insulin resistance in T2DM patients, as it does in nondiabetic patients. However, in T2DM patients, this effect also exaggerates the hyperglycemic response to carbohydrate.
Caffeine can impair glucose regulation in the real world as well as in the laboratory. An ambulatory study monitored glucose levels continuously for several days during the ordinary activities of a small group of T2DM coffee drinkers. The results provide evidence that caffeine impairs glucose regulation in the natural environment where caffeine is consumed, as it does in the laboratory.
Mechanism
In general, caffeine is thought to produce its widespread physiological effects through actions as a potent antagonist for adenosine receptors both centrally and peripherally. One hypothesis is that caffeine impairs glucose metabolism through the release of stress hormones, especially epinephrine and cortisol. Evidence from two human studies supports this hypothesis.
One study found that the drug propranolol, used to block the beta-adrenergic actions of epinephrine, abolished caffeine's exaggeration of the postprandial insulin response and the reduction of whole-body insulin sensitivity.
A second study found that caffeine had no effects on glucose tolerance in a group of adults with tetraplegia, who did not produce increased epinephrine in response to caffeine. Both studies suggest that epinephrine could mediate caffeine's effects on glucose and insulin resistance.
However, a study that directly compared caffeine with high- and low-dose epinephrine infusions for their effects on insulin sensitivity found that caffeine did not raise epinephrine levels high enough to fully account for effects on glucose metabolism.
 |
| Caffeine Content in Beverages |
Although evidence is strong that caffeine produces a transient resistance to insulin action and impairment of glucose tolerance, doubts have been raised about the relevance of these acute effects to the potential public health impact of chronic daily consumption of caffeinated beverages like coffee, tea, and soft drinks.
Perhaps the strongest doubt arises from the common belief that habitual consumption of coffee or other caffeinated beverages leads to the development of tolerance to caffeine and the disappearance of acute effects after daily use. However, there is good reason to believe that habitual caffeine intake does not eliminate the increases in insulin resistance.
A second doubt concerns whether drinking coffee has the same effects as caffeine ingested in capsules. This question is especially relevant given the evidence that heavy coffee drinking is associated with lower risk of developing T2DM. Evidence from studies suggests that coffee has effects similar to pure caffeine. Consumption of coffee, tea, and caffeinated soft drinks may all have similar effects, due to the caffeine that each contains.
A third doubt about the public health relevance of these effects is whether the effects of caffeine on glucose metabolism are sufficiently large to be of clinical importance for the prevention or management of T2DM. Evidence suggests that the effects of habitual caffeine consumption could be large enough to offset at least part of the therapeutic effects of medications commonly prescribed for the management of glucose in T2DM. In addition, caffeine abstinence, as a lifestyle intervention, might yield improvements in chronic glucose control large enough to qualify as a useful adjunctive treatment.
Contradictory Evidence
Although the experimental results clearly indicate that caffeine consumption should be a public health concern for the prevention and management of T2DM, epidemiological studies have reported results that contradict this conclusion. These studies have consistently found that nondiabetic adults who are heavy coffee drinkers, typically four to six cups per day or more, have a lower risk of developing T2DM in subsequent years.
Causal explanations require a plausible mechanism, which has not been established so far for the link between heavy coffee consumption and protection from T2DM. The most common speculation is that one or more of the many compounds in coffee, other than caffeine, is responsible.
This idea is supported by evidence linking decaffeinated coffee consumption to a lower risk of T2DM in some studies. However, research into the effects of these coffee compounds in humans is in its very early stages. It would be premature to assume that these compounds are bioactive and protect against the pathological processes that lead to T2DM.
An alternative interpretation of the epidemiological evidence is that heavy coffee drinking is not the true cause of lower risk, but is simply a marker for another factor that is responsible. After all, individuals select for themselves how much coffee they will consume, and consumption of six of more cups is relatively rare
However, recent research does suggest another possibility that could explain the inverse association of coffee and T2DM risk. Consumption of sugar-sweetened beverages, such as soft drinks, fruit drinks, iced tea, and energy drinks, has recently been associated with an increased risk of T2DM.
Perhaps the strongest doubt arises from the common belief that habitual consumption of coffee or other caffeinated beverages leads to the development of tolerance to caffeine and the disappearance of acute effects after daily use. However, there is good reason to believe that habitual caffeine intake does not eliminate the increases in insulin resistance.
A second doubt concerns whether drinking coffee has the same effects as caffeine ingested in capsules. This question is especially relevant given the evidence that heavy coffee drinking is associated with lower risk of developing T2DM. Evidence from studies suggests that coffee has effects similar to pure caffeine. Consumption of coffee, tea, and caffeinated soft drinks may all have similar effects, due to the caffeine that each contains.
A third doubt about the public health relevance of these effects is whether the effects of caffeine on glucose metabolism are sufficiently large to be of clinical importance for the prevention or management of T2DM. Evidence suggests that the effects of habitual caffeine consumption could be large enough to offset at least part of the therapeutic effects of medications commonly prescribed for the management of glucose in T2DM. In addition, caffeine abstinence, as a lifestyle intervention, might yield improvements in chronic glucose control large enough to qualify as a useful adjunctive treatment.
Contradictory Evidence
Although the experimental results clearly indicate that caffeine consumption should be a public health concern for the prevention and management of T2DM, epidemiological studies have reported results that contradict this conclusion. These studies have consistently found that nondiabetic adults who are heavy coffee drinkers, typically four to six cups per day or more, have a lower risk of developing T2DM in subsequent years.
Causal explanations require a plausible mechanism, which has not been established so far for the link between heavy coffee consumption and protection from T2DM. The most common speculation is that one or more of the many compounds in coffee, other than caffeine, is responsible.
This idea is supported by evidence linking decaffeinated coffee consumption to a lower risk of T2DM in some studies. However, research into the effects of these coffee compounds in humans is in its very early stages. It would be premature to assume that these compounds are bioactive and protect against the pathological processes that lead to T2DM.
An alternative interpretation of the epidemiological evidence is that heavy coffee drinking is not the true cause of lower risk, but is simply a marker for another factor that is responsible. After all, individuals select for themselves how much coffee they will consume, and consumption of six of more cups is relatively rare
However, recent research does suggest another possibility that could explain the inverse association of coffee and T2DM risk. Consumption of sugar-sweetened beverages, such as soft drinks, fruit drinks, iced tea, and energy drinks, has recently been associated with an increased risk of T2DM.
A meta-analysis of the studies reporting this association suggests that those individuals who drink one to two servings per day have a 26% greater risk of developing T2DM than those who drink none, or less than 1 per month.
Common sense suggests that those individuals who are heavy coffee drinkers probably consume little or none of these other beverages. The apparent benefits of coffee drinking may simply be due to an avoidance of the sugar-sweetened alternatives.
Common sense suggests that those individuals who are heavy coffee drinkers probably consume little or none of these other beverages. The apparent benefits of coffee drinking may simply be due to an avoidance of the sugar-sweetened alternatives.
The epidemiological studies have provided new directions for investigation, such as the biological activity of noncaffeine compounds found in coffee. Beyond the potential to discover new chemical compounds, however, their results probably offer little benefit to diabetes prevention and public health.
Premature attributions of cause and effect should certainly not be used to justify recommendations in favor of coffee drinking as beneficial to health, especially given the broad range of adverse effects attributable to caffeine.
Premature attributions of cause and effect should certainly not be used to justify recommendations in favor of coffee drinking as beneficial to health, especially given the broad range of adverse effects attributable to caffeine.